Minnesota Department of Health
 Addressing the three dimensions of the Triple Aim – (1) improving the patient’s experience of care, (2) improving the health of populations, and (3) reducing the per-capita cost of healthcare – is a challenge familiar to health reform initiatives across the country. With healthcare spending in the United States representing a growing and unsustainable share of the economy – projected to hit $3.2 trillion in 2015, according to the U.S. Centers for Medicare & Medicaid Services (CMS) – it is critical that reform activities understand and illuminate the key drivers of spending growth, using data to drive transformative and sustainable changes across systems of healthcare.
Addressing the three dimensions of the Triple Aim – (1) improving the patient’s experience of care, (2) improving the health of populations, and (3) reducing the per-capita cost of healthcare – is a challenge familiar to health reform initiatives across the country. With healthcare spending in the United States representing a growing and unsustainable share of the economy – projected to hit $3.2 trillion in 2015, according to the U.S. Centers for Medicare & Medicaid Services (CMS) – it is critical that reform activities understand and illuminate the key drivers of spending growth, using data to drive transformative and sustainable changes across systems of healthcare.
The State of Minnesota is a pioneer when it comes to turning data into actionable analysis. Leveraging the data from its statewide all-payer claims database (MN APCD), developed and operated by Onpoint since 2009, Minnesota is able to drill into the issues driving the cost of healthcare.
Despite having one of the nation’s most efficient and cost-effective healthcare systems, Minnesotastill must allocate a large share of its economy to maintaining its healthcare-related services and resources. In 2012, the state spent $39.8 billion (13.5 percent of its economy) on such activities – and that number is expected to nearly double by 2022, according to the Minnesota Department of Health (MDH). To curtail the looming affordability challenges for individual consumers, businesses, and other healthcare purchasers, the Legislature recently expanded the authority of the MDH to use the MN APCD for a select number of analytic projects that will investigate the state’s healthcare system to identify possible improvements.
 Among the most recent analyses undertaken by the MDH Health Economics Program is an examination of emergency department (ED) visits and hospital admissions and re-admissions in order to identify potentially preventable healthcare events. The MDH’s newly published report “marks the first time [the MDH and state leaders] have been able to conduct a comprehensive empirical exploration of the volume of potentially preventable health care events in Minnesota and their associated cost.”
Among the most recent analyses undertaken by the MDH Health Economics Program is an examination of emergency department (ED) visits and hospital admissions and re-admissions in order to identify potentially preventable healthcare events. The MDH’s newly published report “marks the first time [the MDH and state leaders] have been able to conduct a comprehensive empirical exploration of the volume of potentially preventable health care events in Minnesota and their associated cost.”
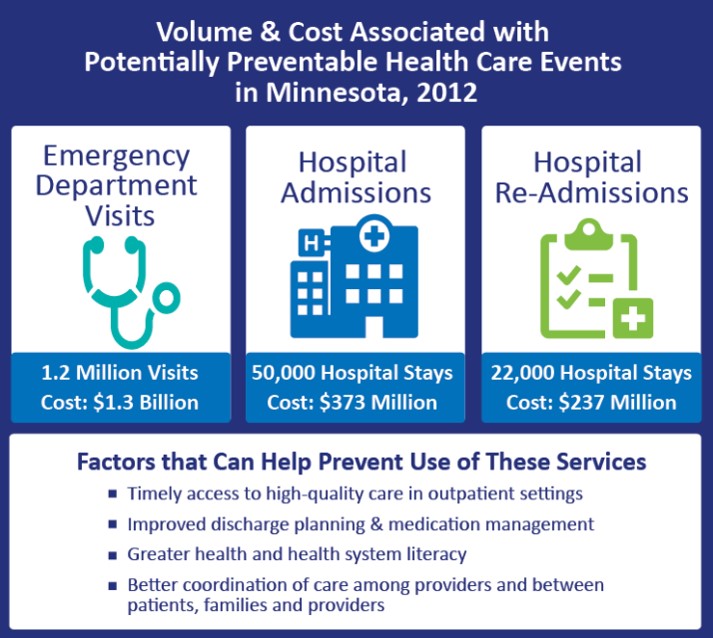
The report, “An Introductory Analysis of Potentially Preventable Health Care Events in Minnesota,” found that Minnesotans experienced an estimated 1.3 million potentially preventable healthcare events in 2012. This volume of potentially preventable services cost private payers and taxpayers approximately $1.9 billion — roughly 4.8 percent of the state’s total healthcare spending in 2012. (It’s important to note that “this volume of spending does not, however, represent real potential savings because not all identified events were actually clinically preventable – on average, cases might be preventable, but individual patient circumstances might make care necessary,” according to the report.)
Below is a summarized look at Minnesota’s potentially preventable outcomes in 2012 by type of healthcare event:
- Emergency room visits: 67 percent of all hospital emergency room visits were potentially preventable, totaling approximately $1.3 billion in healthcare spending.
- Hospital admissions: 10.6 percent of all hospital admissions were potentially preventable, consuming approximately $373 million in healthcare spending.
- Hospital re-admissions: 4.4 percent of all hospital re-admissions were potentially preventable, accounting for approximately $237 million in healthcare spending.
According to State Health Economist and Director of the Health Economic Program at the MDH, Stefan Gildemeister, MA, the MDH’s findings will lead to a more detailed follow-up analysis of health costs in order to try to shift care into lower-acuity settings. Future research efforts aimed at reducing the identified potentially preventable healthcare services will be best focused if “grounded in collaborations with the community, clinical expertise provided by practitioners, and existing delivery system experience with addressing factors associated with potentially preventable health care events,” the report concludes.