New Reporting Released by the Ohio-Kentucky Comprehensive Primary Care Initiative
The Ohio-Kentucky Comprehensive Primary Care (OH-KY CPC) initiative has been working hard – and making great progress – in expanding transparency and accountability across the Greater Cincinnati region by building a regional culture of team-based care coordination and payment transformation.
The region is one of only seven in the United States to have been selected by the Center for Medicare & Medicaid Innovation (CMMI) at the U.S. Centers for Medicare & Medicaid Services (CMS) to offer population-based care management fees and shared savings opportunities to primary care practices in an effort to improve the efficiency and efficacy of healthcare delivery. This CMMI-funded project spans Medicare, Ohio Medicaid, and seven commercial insurance plans that have agreed to provide data for 75 participating primary care practices representing more than 250 physicians. Participating practices are located across counties in southwest Ohio and north-central Kentucky.
Since the initiative’s inception in April 2012, the Health Collaborative has served as the program’s convener. This Greater Cincinnati-based health care improvement nonprofit organization has been providing leadership and fostering collaboration among participating payers and providers. To guide their efforts, the Health Collaborative has partnered with Onpoint to build a multi-payer claims database that spans data collection, integration, enhancement, performance measurement, analysis, and reporting.
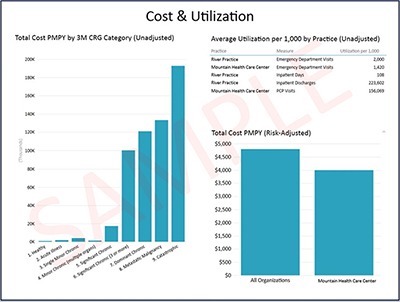
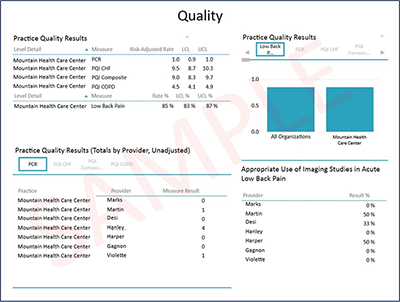
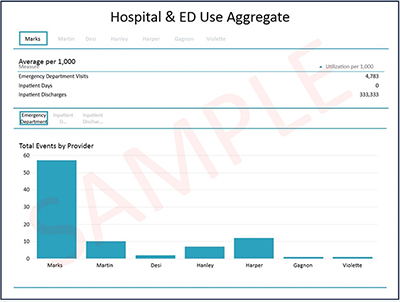
The Health Collaborative recently released the initiative’s first set of dynamic reports to participating public and private payers and their primary care practices. This reporting, developed collaboratively using dynamic pivot tables, end users to quickly summarize and present aggregate and patient-level data in the form of interactive visualizations that facilitate comparative analyses of patterns and trends. This reporting specifically seeks to help inform potential downstream opportunities for care delivery and payment reform improvement.
For each report, data is broken down into 10 different subject areas that feature reporting across multiple measures, including expenditures (e.g., total cost of care, primary care cost), quality (e.g., ambulatory care sensitive condition admissions, HEDIS plan all-cause readmissions), and utilization (e.g., inpatient discharges, outpatient emergency department visits). Measures were risk adjusted, accompanied by 95% confidence intervals, and capped for outliers to avoid distortion.
Follow-on reporting for the OH-KY CPC initiative will be released on a quarterly schedule, with the next round scheduled for distribution in late May. In addition to the data supplied by each of the participating commercial payers, anticipated data sources include Ohio Medicaid and CMS’s Medicare fee for service (FFS), providing an even broader view of the healthcare services being delivered across the region.